3B: Management
This section covers:
Management strategies
Once you have identified the signs and symptoms of a venous leg ulcer, you then need to determine the appropriate treatment. Key evidence based management strategies for venous leg ulcers include the following:
| Strategy | Explanation |
| Use suitable dressings | Dressings used to treat venous leg ulcers vary depending on the condition of the ulcer and the goals of treatment. Dressings should maintain a moist wound-healing environment, manage wound leakage (exudate), protect the skin around the ulcer, be non-adherent to reduce trauma on removal, be cost-effective, be acceptable to the client and be able to be changed less often where possible. |
| Apply graduated compression bandaging | The key to healing a venous leg ulcer is to treat the underlying cause (i.e. reduce the high blood pressure in the veins).
Graduated compression bandages apply pressure to the lower leg to improve the blood flow back to the heart. Bandages are applied from the base of the toes to just below the knee. The bandage is said to be graduated because the ankle is smaller than the calf. Therefore, the pressure exerted by the bandage at the ankle is higher than that applied at the calf. Graduated compression bandaging works by:
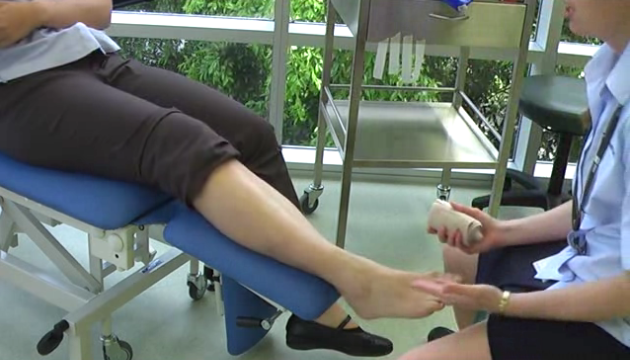
You need special training in how to apply graduated compression bandages correctly because if they are applied incorrectly, they can cause significant damage to the client’s circulation and may even make the ulceration worse. IMAGE - M3 15 Compression bandage |
| Apply compression stockings | Graduated compression stockings for life after wound healing help to prevent venous leg ulcers from recurring, because they continue to provide compression to treat the underlying cause of the leg ulcers (i.e. poor circulation). A venous leg ulcer is really a symptom of an underlying disease process.
Note that compression stockings can also be used to prevent venous leg ulcers and this will be described in section 3C: Prevention. IMAGE - M3 16 Compression stocking |
Applying a compression bandage
Failure to reach an accurate diagnosis and/or to recognise the signs and symptoms of venous disease may result in the unsafe application of the graduated compression bandaging.
Factors that need to be considered before applying graduated compression bandaging include:
| Factor | Explanation |
| Skin condition | If the person has delicate, easily damaged skin, high compression bandages may make these symptoms worse. |
| Shape of the lower leg | If the person has a very small ankle and a very large calf muscle (i.e. inverted champagne bottle-leg appearance), the pressure applied by the bandage may be too high at the ankle so the skin may be damaged by this pressure. IMAGE - M3 17 Champagne bottle leg appearance |
| Lack of sensation | If a person has decreased sensation in their feet or lower limbs, they may not be able to determine if the bandage is too tight, increasing the risk of pressure damage. |
| Heart disease | If the person has a known history of cardiac disease and has very swollen lower legs, applying compression bandages to the lower leg may result in a rapid shift of fluid from the legs back towards the heart. This can be very dangerous and may result in heart failure. |
Characteristics of compression bandages
There are many different types of compression bandages and compression stockings available that you could use to treat venous leg ulcers. As a general rule, compression bandages should have the following characteristics:
| Characteristics | Explanation |
| Is clinically effective | You need to know if the bandage you have selected is supported by evidence based guidelines. Refer to the Guidelines Summary for further information in 3E: Module Resources. |
| Sustains compression | The compression bandage should be able to provide and maintain clinically effective levels of compression for at least one week during walking and rest periods. |
| Enhances calf muscle pump function | The bandage needs to be applied from the toe to the knee to enhance the function of the calf muscle pump. |
| Ease of application | The bandage should be easy to apply and remove. Furthermore, you must be trained in how to successfully apply a graduated compression bandage. The following short video provides an example of how to apply a simple bandage. VIDEO - M3_V01 Bandage application (View video transcript) |
| Is conformable and firm | The bandage should conform to the shape of the person’s lower limb and should be firm but not tight. |
Now that you have learned how to recognise the signs and symptoms of a venous leg ulcer and some management strategies, you are ready to learn about how to prevent leg ulcers from recurring.
Top of page