Glossary
Links
Resources
3C: Prevention
This section covers:
Prevention strategies
Once you have learned how to assess and manage a venous leg ulcer, there are some important evidence based strategies that you can put in place to reduce the risk of the leg ulcer recurring. These include the following:
| Strategy | Explanation |
| Use graduated compression stockings |
|
| Recommend a medical review |
|
| Follow up and check the client’s skin regularly |
|
| Encourage the client to exercise |
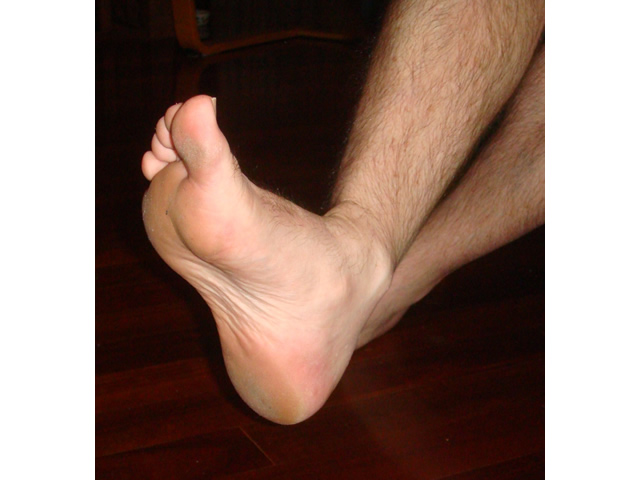
IMAGE - M3 19 Toes to nose IMAGE - M3 20 Toes to floor |
| Elevate the client’s leg |
|
| Ensure the client avoids crossing his/her legs |
|
Tips for using graduated compression stockings
For graduated compression stockings to be effective there are few simple things that you need to consider. These include:
| Considerations | Tip |
| Ladders, tears or holes in the stockings | If the compression stocking has a ladder, tear or hole, this reduces the level of compression provided by the stocking. |
| Bruising or broken skin | If compression stockings are not applied correctly, they can damage the skin, particularly the shin, as they are pulled on. |
| Swelling above and below the stockings or toes purple/blue | If a person complains of swelling above or below the stocking or their toes turn blue or purple, this may indicate that the stocking is too tight and must be removed. |
| Extreme pain, particularly in the foot or calf muscle | Stockings should feel comfortable and be firm but not tight. If a person complains of extreme pain in the foot or calf muscle that they have not experienced previously, this indicates the stocking is too tight and must be removed. |
| Difficulty with applying and removing stockings | It is recommended that clients take off the stockings at night and reapply them first thing in the morning. However, this may not be practical for some people and assistance may be required.
Compression stockings are not put on like ordinary hosiery. If you roll the stocking up to apply, it gets tighter and tighter because the compression starts at the ankle. |
| Encouraging independence | Teaching clients how to apply their stockings is essential to improve their independence. |
| The stocking has wrinkles | Wrinkles should be removed to reduce the risk of the stocking being too tight or slipping down. |
| Stockings folded over at the top | Folds in the stocking can cause problems. For example, tight bands at the top or over the foot may lead to pressure damage or more ulcers. |
| Using a moisturiser | Apply a pH neutral moisturiser to keep the skin in good condition but allow it to dry before applying the stocking. |
| Wearing jewellery when applying and removing stockings | Remove your rings, watch and jewellery as these can damage the stocking. |
| Wearing rubber gloves | It is recommended that you wear rubber dishwashing gloves when applying the stockings to make it easier to grip the stocking and help prevent holes, tears and ladders. IMAGE - M3 22 Rubber gloves |
| Using applicators | There are a variety of stocking applicators such as frames, slide sheets or sockets that can be used to help put stockings on more easily and to avoid trauma to the skin during application. The short video clips show stocking application and removal techniques. IMAGE - M3 23 Stocking applicator VIDEO - M3V02 Stocking application (View video transcript) VIDEO - M3V03 Removal of stocking (View video transcript) VIDEO - M3V04 Application of open-toe stocking (View video transcript) VIDEO - M3V05 Application of close-toe stocking (View video transcript) |
Top of page