1A: Assessment
This section covers:
Functions and layers of the skin
As people start to age, they are more likely to have problems with their skin and wounds (such as skin tears, leg ulcers and pressure injuries) become a fairly common problem. Having a good understanding of the functions of normal skin and the layers of the skin is important so that you are able to recognise risk factors for poor skin integrity. You are then able to undertake actions to prevent skin breakdown or to improve wound healing outcomes for older people.
The skin is the largest organ of the body and maintaining skin integrity is a complex process and one that is often taken for granted until damage occurs. As outlined in the following table, the skin has to perform many different functions.
| Function | Explanation |
| Protection | The skin provides a covering that is designed to protect us from damage or injury. |
| Temperature control (thermoregulation) | As your body sweats, the sweat evaporates and cools the skin. Blood vessels also dilate (or widen) and constrict (narrow) to prevent heat loss and maintain a stable body temperature. |
| Sensation and communication | Nerve endings and receptors are found in the skin and these help us to respond to touch, pain, heat or cold. |
| Metabolism | The skin helps us to metabolise Vitamin D through exposure of the skin to sunlight. |
| Elimination | The skin helps us to eliminate waste through its function of excretion (e.g. sweat) and secretion (e.g. oil). |
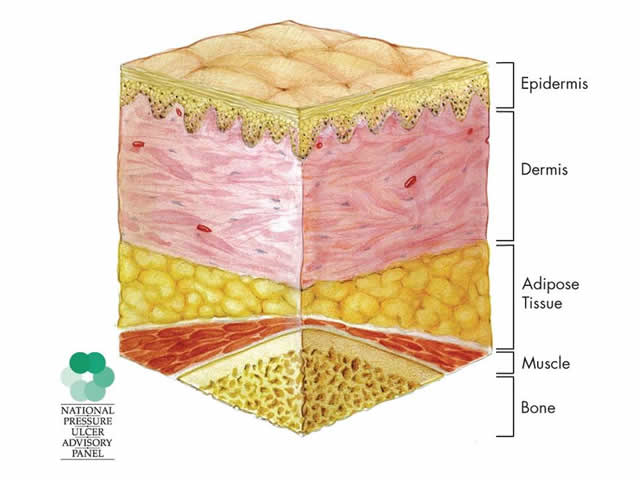
When an injury occurs to the skin, the depth, severity and number of layers damaged by the injury affect how quickly the body is able to repair itself. The thickness of the skin ranges from 0.05-0.3mm depending on location. The thickest skin is on the soles of the feet and the palms of the hands. The thicker the skin the better it is able to withstand injury.
The skin consists of three main layers:
- Epidermis (outermost layer of the skin)
- Dermis (middle layer)
- Subcutaneous layer or "Adipose Tissue" (bottom layer of the skin).
Top of page
Skin changes associated with ageing
Many older people have problems with their skin, therefore it is very important to be able to recognise the common characteristics of ageing skin.
There are two types of skin ageing:
- Intrinsic ageing - all people experience alterations in the structure and function of the skin due to normal maturity.
- Extrinsic ageing - some people experience ageing due to constant or repeated exposure to environmental elements such as the sun.
Ageing caused by these internal and external factors is further explained below:
| Type of problem | Explanation |
| Decreased sensory perception | This means reduced sense of touch and pain, so that when an older person injures their skin, they may not be aware they have done so. Example: When an older person gets a skin tear, they may not realise until they see the injured body part. IMAGE - M1 02 Skin tear |
| Increased dryness | The skin becomes drier and less supple because sebaceous and sweat gland activity decreases with age. Example: Many older people complain of dry, itchy skin. |
| The skin becomes thinner and less elastic | The skin decreases in turgor or thickness because of reduced collagen and elastic fibre production. The collagen present becomes thinner and when combined with less adipose or fatty tissue, the skin support structure is compromised so skin wrinkling occurs. Such skin is subject to friction and shearing trauma. The skin on the back of the hands becomes thin and transparent, whilst the skin on the back of the neck has a furrowed appearance. Example: Ageing skin has more risk of skin tears, bruises and lesions as a result of thinner, less flexible skin and a lifetime of exposure to the sun. IMAGE - M1 03 Poor skin turgor |
| Decreased vitamin D synthesis | This is often due to inadequate exposure to sunlight, decreased dietary intake of Vitamin D or a medical condition. Example: It may take longer for skin to repair and older people have an increased risk of fractures. |
| Reduction in immune response | Cells which trigger the immune system are slower to respond and less effective. Example: There is an increased risk of infection for even minor skin injuries. |
| Decrease in temperature control or thermoregulatory functioning | Older people are less able to regulate their body temperature due to changes in environmental temperature. Example: Some older people may complain of being cold even on a hot day. |
| Vascularity or blood supply of the skin is diminished | Blood vessels in the dermis become fragile and there is decreased peripheral circulation (i.e. less blood flows to the skin and extremities). Example: Older people bruise easier. Also, their fingernails lose their lustre and toenails thicken. IMAGE - M1 04 Thickened toenails |
| Hormonal changes | Facial hair in males decreases and yet increases in females. Pubic and axillary hair thins, straightens, greys and lessens because of reduced hormonal functioning. Both males and females experience overall hair loss from the trunk and extremities. Hair loss on the lower limbs may also occur when peripheral vascular disease is present. Hormonal changes also lead to drier skin. |
| Changes in hair colour and balding | Scalp hair greys and balding occurs because of a reduction in the number and functioning of melanocytes, the cells which give hair and skin their colour. The density and rate of scalp hair growth also declines and the size of hair follicles increases leading to baldness. IMAGE - M1 05 Greying hair & skin wrinkling |
| The amount of subcutaneous tissue decreases | The amount of subcutaneous tissue decreases particularly in the extremities. Example: Joints and bony prominences have a sharp, angular appearance. The hollows in the thoracic (chest), axillary (under the arms) and supraclavicular (collar bone) regions deepen. IMAGE - M1 06 Hollow under arm |
How to assess the skin
Being able to recognise changes associated with ageing enables you to use appropriate strategies to prevent skin breakdown. When undertaking an assessment of the skin, there are three important steps that you should take to be able to identify all of the risk factors.
Step 1: Prepare the environment
Firstly, you need to create an environment that is suitable to conducting an assessment by:
- ensuring that the room is quiet, private and has a stable temperature. This helps to reduce anxiety
- ensuring adequate lighting so that you can see the colour of the skin or any skin changes
- ensuring adequate exposure of the skin, especially areas not usually inspected such as the buttocks, axillae (armpits), back of thighs or feet.
Step 2: Gather relevant information
Secondly, you need to explain what you are going to do and the purpose of assessing the skin. Typically, you obtain information in the order shown here:
| Information required | Questions you might ask a client |
| Past medical history | Tell me what other health conditions you may have? Example: Diabetes may lead to loss of sensation in the feet and an inability to feel if an injury has occurred. |
| Medications (topical, systemic, over-the-counter) | Are you taking any medications that might affect your skin? For example, medications that might make the blood thinner (anticoagulants) or steroids (taken for conditions such as rheumatoid arthritis). Example: Skin tears are common injuries in people who take blood thinning drugs or steroids. |
| Exposure to environmental or occupational hazards | What sort of work did you do? Were you exposed to the sun a lot when you were younger? |
| Substance abuse | Do you smoke or have you ever smoked? How much did you smoke? When did you stop smoking? How much alcohol intake do you have? Have you ever used illicit drugs? Example: Fingernails are often stained yellow by nicotine exposure. IMAGE - M1 07 Nicotine stained fingernails |
| Recent physiological or psychological stress | Have you experienced a recent stressful event? Have you been unwell recently? How does this affect you? |
| Hair, nail and skin care habits | What methods do you use for cleansing your skin? How often do you moisturise? How do you dry your skin? Example: Many soaps, oils, lotions, cosmetics and home remedies have preservatives that can irritate the skin and make it itchy or inflamed. |
| Skin self-examination | How often do you look at your skin? Are you able to see your skin properly? Can you reach to dry between your toes? |
| Problems with the skin | Have you noticed any changes in your skin (e.g. dryness, rashes, lumps, amount of perspiration), when did the symptoms occur? Are these symptoms new or an old problem? What area of the body is affected (i.e. skin folds, localised or generalised)? Are there any associated symptoms (e.g. fever, relationship to stress or leisure activities) and what have you been doing for the problem? Example: Eczema is a common problem that is often made worse by some creams and it may be a lifetime problem for that person. Careful questioning will help to determine what the person has been doing to treat the condition, what works for them and what doesn’t work to treat the problem. |
Step 3: Observe and feel the skin
The final step is to look at the skin (inspection) and feel (palpation) if there are any changes.
| Observations | Explanation |
| Skin temperature | If the skin around a wound is very hot to touch compared to the surrounding skin, this may indicate an infection. If the feet are abnormally cold to touch, this may indicate a problem with circulation. |
| Skin texture | You need to consider different types of textures such as rough, coarse, fine, flaky, scaly or smooth. Example: Rough skin may indicate that the skin is very dry. |
| Skin colour | The colour of the skin (e.g. pink, red, blue, pale or yellow) can indicate a person’s general wellbeing. Example: A person whose lips and mucous membranes are tinged blue may indicate a heart problem. Yellow skin can indicate a problem with the liver. |
| Skin changes | The presence of growths, discolouration, infections, broken areas, old scars, rashes, eczema, dermatitis, senile purpura, cherry angiomas, thickened skin may be normal changes associated with ageing or indicate a person’s risk of a wound recurring. IMAGE - M1 08 Senile purpura |
| Turgor (resilience and elasticity of tissue) | Skin turgor can give an indication of the person’s nutrition and hydration status. |
| Hair distribution, colour and quantity (thick, thin, balding) | Uneven hair loss may indicate a person’s psychological state. Example: A person may unconsciously pull their hair out if they are traumatised. |
| Nail length, colour, configuration, symmetry and cleanliness | The colour of a person’s fingernails may indicate certain problems. Example: Fingernails stained yellow indicate nicotine use. Blue fingernails can indicate a problem with circulation such as heart or respiratory disease. |