3A: Assessment
This section covers:
What is a leg ulcer?
A leg ulcer is a wound that occurs between the knee and ankle that takes more than four weeks to heal. There are two common types of leg ulcers: venous and arterial leg ulcers. In this module you will learn about venous leg ulcers.
Assessment is the key to effective management of leg ulcers, yet many people with leg ulcers have never had a specialist assessment to identify the type of leg ulcer they are suffering from. Hence, leg ulcers may last for many years and even if they heal, they may soon break out again if the correct treatment and prevention strategies have not been provided.
Top of pageVenous leg ulcers
Venous leg ulcers are the most common type of leg ulcer. They occur because of high blood pressure in the veins in the lower limb (known as “venous hypertension”). Veins carry blood from the legs back to the heart. Veins in the lower leg have one-way valves to prevent blood running backwards and when the calf muscles contract, blood is moved along the veins back towards the heart.
However, sometimes the valves in the veins or calf muscle fail to work properly for a number of different reasons (e.g. damage from a past clot in the vein), leading to chronic venous insufficiency or venous disease. The constant high pressure in the veins eventually causes fluid to leak out of the veins and into the surrounding tissues and skin. Although the reason for ulcer formation is not fully understood, the combination of high pressure in the veins and particles in the fluid forced into the tissues causes inflammation. This results in the skin easily breaking down and forming an ulcer.
Top of pageRisk factors
Typical risk factors are explained further in the following table.
| Risk factor | Explanation |
| Age | Blood flow decreases as you age and decreased mobility is associated with the calf muscles becoming less effective. |
| Obesity | Excess weight, particularly around the waist and thighs, puts extra pressure on the veins and they have to work harder to move blood flow back towards the heart. Note that multiple pregnancies may also be a cause of excess weight. |
| Varicose veins | The one-way valves that stop blood from travelling backwards in the veins stop working and this leads to pooling of blood in the lower legs. |
| Past deep vein thrombosis or trauma to lower limbs | A history of deep vein thrombosis (i.e. blood clot) or trauma may result in permanent damage to the veins. |
| Jobs that involve sitting or standing for long periods of time | Occupations that involve sitting or standing for long periods of time may result in less effective blood flow through the veins and pooling of blood in the lower legs. |
| Family history or congenital valvular incompetence | There is a strong link between family history and leg ulcers. In addition, in rare cases some people are born with problems that affect their veins placing them at higher risk of venous disease. |
| Health conditions | Disorders such as congestive cardiac failure lead to swelling of the lower limbs because the heart is not able to process blood flow effectively. |
Characteristics
Every leg ulcer has key features or characteristics that help us to determine the type of leg ulcer the person is suffering from. The key characteristics of venous leg ulcers are outlined in the following table.
| Characteristic | Venous leg ulcer details |
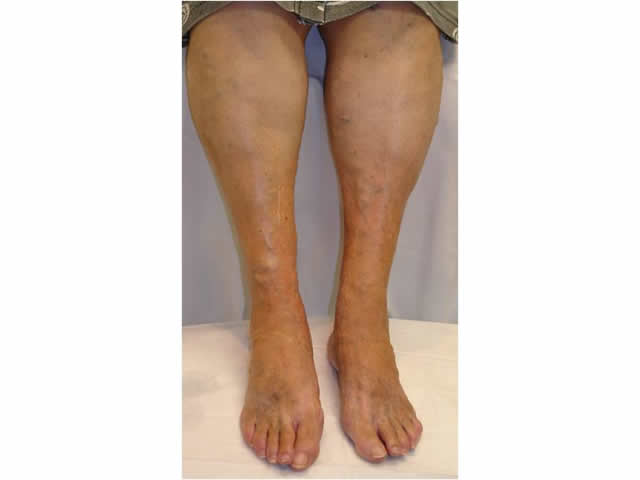
| Wound location | Venous leg ulcers are located above the ankle bones, on the lower third of the leg in the calf muscle region. IMAGE - M3 01 Venous leg ulcer |
| Wound depth | Venous leg ulcers are usually shallow affecting the epidermis and dermis. |
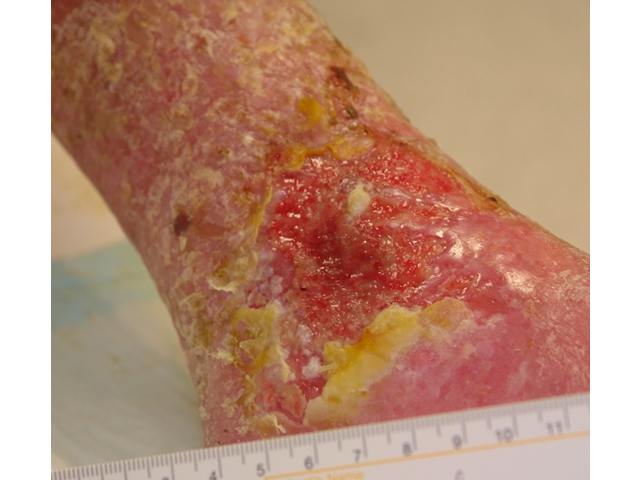
| Appearance of wound bed | The wound bed is often described as having a ruddy or beefy red, granular appearance. IMAGE - M3 02 Appearance of venous leg ulcer wound bed |
| Wound shape and margins | The wound margins are flat and irregular, often resembling the shape of a cartoon figure or country. IMAGE - M3 03 Flat, irregular wound margin |
| Wound leakage (also known as “exudate”) | Venous leg ulcers leak moderate to heavy amounts of liquid. |
| Surrounding skin | The surrounding skin has many characteristics that help us to categorise the leg ulcer as one of venous origin, including:
|
| Pain levels | Pain levels range from no pain to severe, constant pain. Pain is often worse after standing for long periods. It may be described as an achy, dull pain or a feeling of pressure. Pain is usually relieved by elevating the limb above heart level, because this relieves the pressure on the veins and reduces swelling. |
How to assess
Being able to recognise the key signs and symptoms of a venous leg ulcer is very important to help diagnose a venous leg ulcer accurately. However, there are several important steps that must also be performed. These include:
| Step | Explanation |
| 1. Obtain the client’s health history | This includes a history of the present leg ulcer or symptoms. You might like to ask:
It is also important to ask about general health and medical conditions the person may have such as smoking history, mobility, medication and nutritional status. |
| 2. Examine the client’s legs | Look at the legs and note if there is any swelling. You need to be able to answer these questions:
Also, measure the ankle and calf circumference because once you start treatment, you need to know if there is any reduction in the size of the ankle and calf over time. |
| 3. Examine the client’s foot pulses | You need to palpate (touch) foot pulses, particularly the pulse located on top of the foot (known as the “dorsalis pedis pulse”). If this pulse feels strong on palpation , this indicates good blood flow to the lower limb. |
| 4. Examine the ulcer | Measure the size of the ulcer at least every four weeks or if there is any rapid improvement or deterioration in wound size. This helps to determine if your treatment is working or not.
Note the presence of any smell, the colour of the wound bed, how much exudate or leakage the wound is producing and condition of surrounding skin. Also, note characteristics of the wound margin. Venous leg ulcers have sloping wound margins that are irregular in appearance. |
| 5. Measure the Doppler Ankle Brachial Pressure Index (ABPI) | A trained health professional should carry out a hand-held Doppler Ankle Brachial Pressure Index (ABPI) examination. This involves first performing a blood pressure test on both arms and both legs and listening to the arteries with an ultrasound machine, and then comparing the ankle and brachial systolic pressures. This test helps to determine the type of treatment the client may need or if they need to be referred to a specialist for further investigation. |
When to refer
It is very important that you refer the client to a specialist in these circumstances:
- There is uncertainty in the diagnosis (i.e. it is difficult to determine the type of ulcer based on clinical signs and symptoms alone)
- There is a low or high Ankle Brachial Pressure Index (ABPI) (i.e. less than 0.9 or greater than 1.2)
- The ulcer is complicated (e.g. multiple aetiology such as arterial, rheumatoid disease)
- There are signs of infection
- The ulcer deteriorates
- The ulcer fails to improve after 3 months.
Top of page

M3 01 Venous leg ulcer

M3 02 Appearance of venous leg ulcer wound bed

M3 03 Flat, irregular wound margin

M3 04 Ankle flare

M3 05 Telegectasia or ankle flare
M3 06 Varicose veins

M3 07 Swelling of the lower leg

M3 08 Atrophie blanche above ulcer

M3 09 Maceration

M3 10 Hyperpigmentation
M3 11 Hyperkeratosis

M3 12 Venous stasis eczema

M3 13 Haemosiderin staining

M3 14 Lipodermatosclerosis


